The COVID-19 pandemic is hitting racial minority groups, particularly the African American community, harder than white people. Historically, racial minorities are more heavily impacted by pandemics and other health crises. Racial/ethnic minority populations experience worse health outcomes during and after these disasters. This is often due to more underlying health conditions, living conditions, lack of access to health care, cultural/language barriers, and inadequate access to educational resources.
Members of racial/ethnic minority groups often live in densely populated areas, such as large cities or households with many people, which can make it difficult to adequately practice social distancing. Additionally, many of these groups are living far away from medical facilities, which makes it harder to seek testing or treatment when sick. Furthermore, these individuals frequently work in essential jobs such as grocery stores, are being exposed to the virus and don’t have the option to stay home. They also typically have a higher prevalence of chronic conditions and less access to health care due to lack of insurance or distrust of the medical system. This fundamental distrust of the healthcare system stems from cultural, financial and language barriers associated with receiving care. The COVID-19 pandemic has brought a lot of these systemic issues to light, emphasizing the problems with racial inequity within the health care system.
Source: https://www.datacenterresearch.org/covid-19-data-and-information/covid-19-data/
African American and Hispanic individuals are being infected and dying at an alarming rate. In Louisiana, a state hit particularly hard at the beginning of the pandemic, 70% of COVID-19 related deaths were African American individuals, despite them only making up 32% of the state’s population. A similar pattern of mortality rates can be seen in other large cities such as New York, Chicago, and Washington DC.
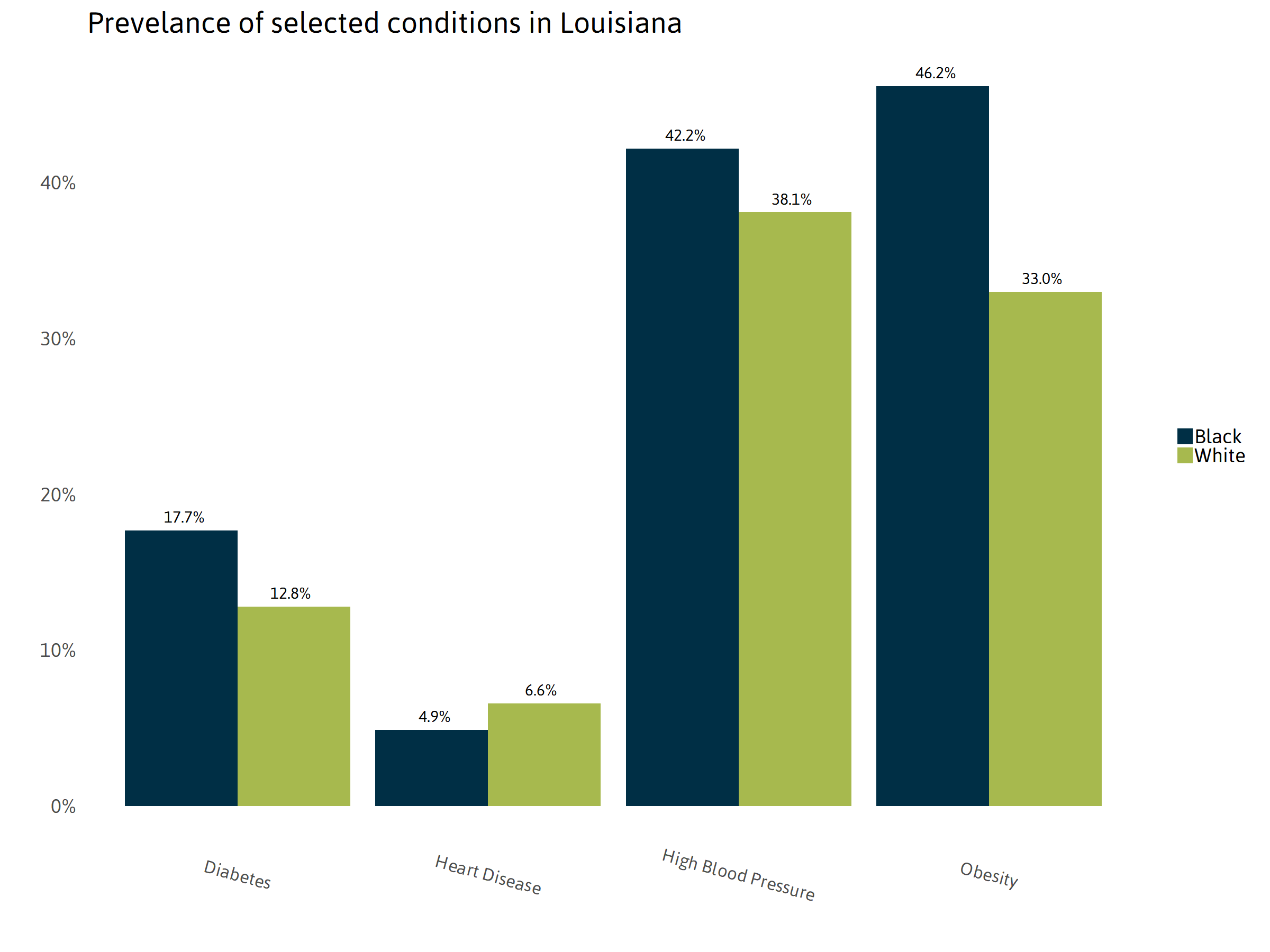
People of color typically have higher rates of pre-existing conditions that become risk factors for COVID-19. Conditions such as diabetes, heart disease, obesity, and hypertension are more prevalent in communities of color. These conditions are also associated with increased mortality rates and other complications when contracting COVID-19. Many of these underlying health conditions are due to socioeconomic difficulties. Living far away from a grocery store or being unable to access health care can lead to some of these underlying health conditions.
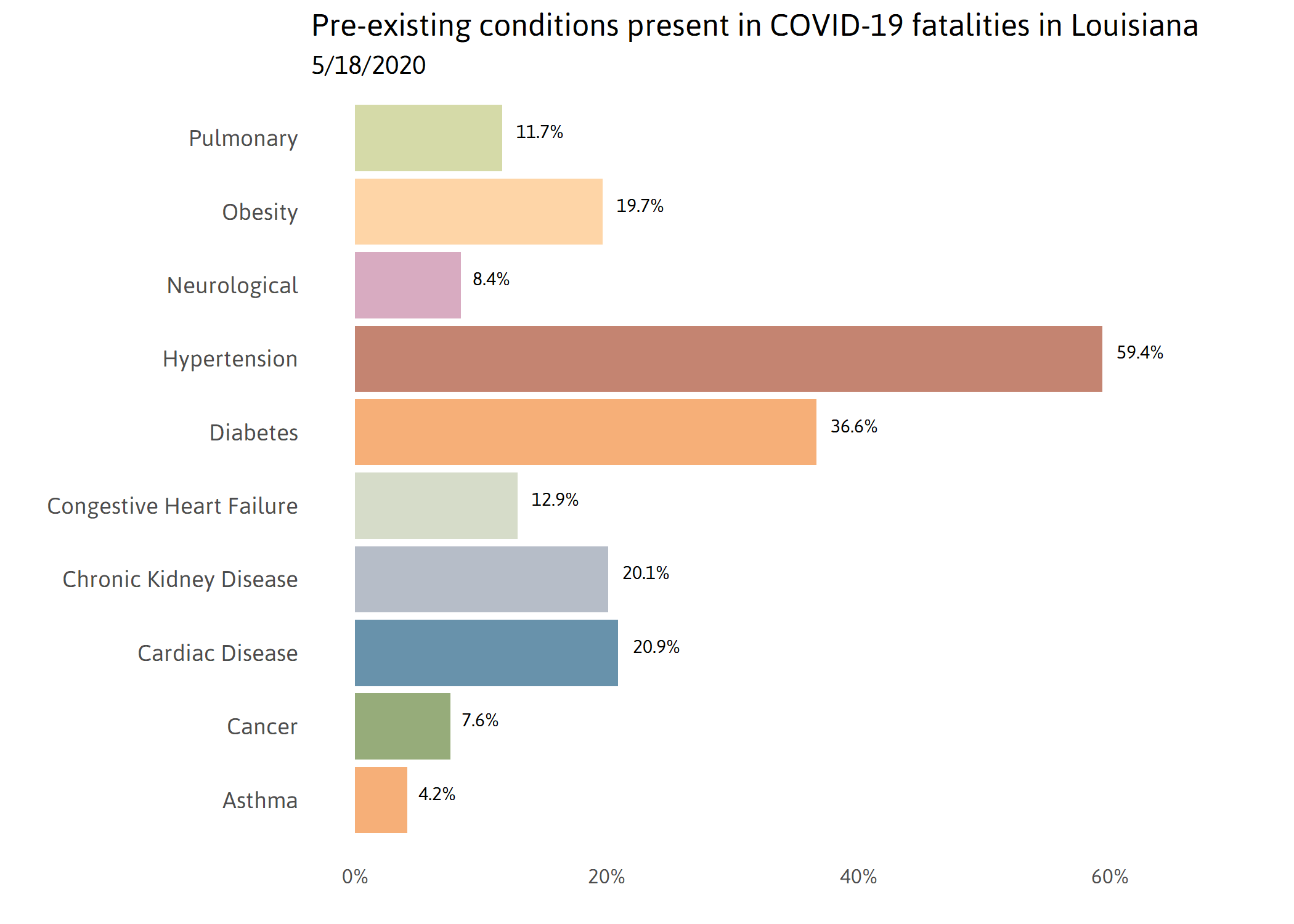
Source: https://www.datacenterresearch.org/covid-19-data-and-information/covid-19-data/
Another major factor contributing to higher rates of COVID-19 among minority groups is living and working conditions. African American and Hispanic individuals often work in essential, in-person jobs and cannot stay home which makes them more likely to contract COVID-19. Additionally, they also often live in crowded, densely populated areas which makes it easier for COVID-19 to spread through the community. Many individuals also live in multi-generational homes, with elderly parents and grandparents who are more susceptible to complications due to COVID.
Limited access to health care also contributes to worse health outcomes from the COVID-19 pandemic. Many minorities live further away from health care facilities, like hospitals and testing sites, which makes it harder to seek care. Inadequate access to health care stems from a fundamental distrust of the health care system, cultural and language barriers, and financial implications. Lower access to health care makes it difficult for people to seek treatment when sick and limits access to testing centers. Furthermore, many minority groups are not receiving information about testing and treatment, potentially due to language barriers.

Cherice Harrison-Nelson, aka Queen Reesie
I had the opportunity to interview New Orleans native Cherice Harrison-Nelson about her personal thoughts and experiences on health disparities during the COVID-19 pandemic. A short video with our conversation can be viewed here.
The COVID-19 pandemic, like many other pandemics historically is negatively impacting racial minority groups at a significantly higher rate than others. These health disparities have been seen for many years and are being highlighted by the current pandemic. African American and Hispanic individuals are being infected and dying at an alarming rate. In order to address these disparities government and health officials need to understand where the disparities are coming from, and work to change the systems currently in place. Providing economic support for individuals who need to stay home, increasing education, and increasing access to health care services are some steps that the US should be taking to reduce these disparities and help slow the impact of COVID-19 on minority communities. Getting rid of the systemic inequity with significant policy change is the only way to reduce these disparities and protect minority groups from the next pandemic or other health crises.
Sources:
Quinn, Sandra Crouse, and Supriya Kumar. “Health Inequalities and Infectious Disease Epidemics: a Challenge for Global Health Security.” Biosecurity and Bioterrorism : Biodefense Strategy, Practice, and Science, Mary Ann Liebert, Inc., 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4170985/.
Quinn, Sandra, et al. “Racial Disparities in Exposure, Susceptibility, and Access to Health Care in the US H1N1 Influenza Pandemic.” American Public Health Association (APHA) Publications, Sept. 2011, ajph.aphapublications.org/doi/abs/10.2105/AJPH.2009.188029.
Alcendor, Donald J. “Racial Disparities-Associated COVID-19 Mortality among Minority Populations in the US.” Journal of Clinical Medicine 9.8 (2020): Journal of Clinical Medicine, 30 July 2020, Vol.9(8). Web.
Raifman, Matthew A, and Raifman, Julia R. “Disparities in the Population at Risk of Severe Illness From COVID-19 by Race/Ethnicity and Income.” American Journal of Preventive Medicine 59.1 (2020): 137-39. Web.
 NOLAbeings
Multimedia artist Claire Bangser created NOLAbeings as a portrait-based story project that marries...
NOLAbeings
Multimedia artist Claire Bangser created NOLAbeings as a portrait-based story project that marries...
 Data corner: Adobe Suite (create a PDF, social media graphic, presentation, edit a photo and video
Data corner is where you go to work with analytics and top tech skills. It takes on everything from PERL and SQL to Canva and Sprout Social.
Data corner: Adobe Suite (create a PDF, social media graphic, presentation, edit a photo and video
Data corner is where you go to work with analytics and top tech skills. It takes on everything from PERL and SQL to Canva and Sprout Social.
