It is an understatement to say that New Orleans is one of the strongest and most resilient cities when it comes to crises. There have been multiple disasters from which the city has bounced back after, including Hurricane Katrina and the COVID-19 pandemic. However, there is one health crisis this town is still having trouble shaking off. Human Immune Deficiency Syndrome (HIV) is a sexually transmitted disease that unhinged the United States and the world starting in the 1980s. The disease was first observed in gay men in the United States, creating the misperception that it must originate i n same-sex activities, which was later ruled out by evidence of the disease in women and children. The epidemic of HIV is one of scary proportions because of its ability to progress to Acquired Immunodeficiency Syndrome (AIDS), which causes severe damage to the immune system and various cancers. Today more than 1 million people are living in the United States with HIV, and over 56,000 new cases are presented each year. Black populations represent a disproportionate ratio of these cases with an estimated population of 468,500 living with HIV, and new diagnoses are 8 times more likely to be black. These disproportions are the reason the Southern states have a much higher percentage of HIV and AIDS cases than other parts of the country.
n same-sex activities, which was later ruled out by evidence of the disease in women and children. The epidemic of HIV is one of scary proportions because of its ability to progress to Acquired Immunodeficiency Syndrome (AIDS), which causes severe damage to the immune system and various cancers. Today more than 1 million people are living in the United States with HIV, and over 56,000 new cases are presented each year. Black populations represent a disproportionate ratio of these cases with an estimated population of 468,500 living with HIV, and new diagnoses are 8 times more likely to be black. These disproportions are the reason the Southern states have a much higher percentage of HIV and AIDS cases than other parts of the country.
Louisiana continuously leads the U.S. with growing HIV numbers. Specifically, the number of HIV cases in New Orleans continues to increase, even though the number of new cases has begun to decrease (Poche). “Dr. Jason Halperin, a physician at New Orleans health clinic CrescentCare, says a major reason of the decline in new cases [is] the development of a preventative drug – (PrEP)” (Poche). Sadly, however, only a small portion of New Orleanians who engage in high-risk behaviors for contracting HIV are taking PrEP. The unequal rates among communities at the highest risk of contracting HIV and access to PrEP are Blacks and people living in the South. According to the Louisiana Department of Health, Blacks living in Louisiana are more than six times more likely to be diagnosed with HIV compared to whites.
The example in New Orleans of people of color heavily affected by HIV and AIDS speaks to the change the route of the disease, the country, and the healthcare system has taken regarding the disease’s treatment. The narrative of HIV is no longer the white gay male in California or New York. The system previously focused on what the problem was in the 80s and 90s, which was vastly different from today’s HIV crisis, largely a Black man’s disease (Villarosa). This problem in New Orleans is rooted in the racism and inequality found in a state with many other prevalent racial issues. Evidence points to hard statistics that prove that Black men are less likely to engage in behaviors that increase contraction; instead, the high rates of infection in Black men point to “systemic barriers tied to racism” (Poche).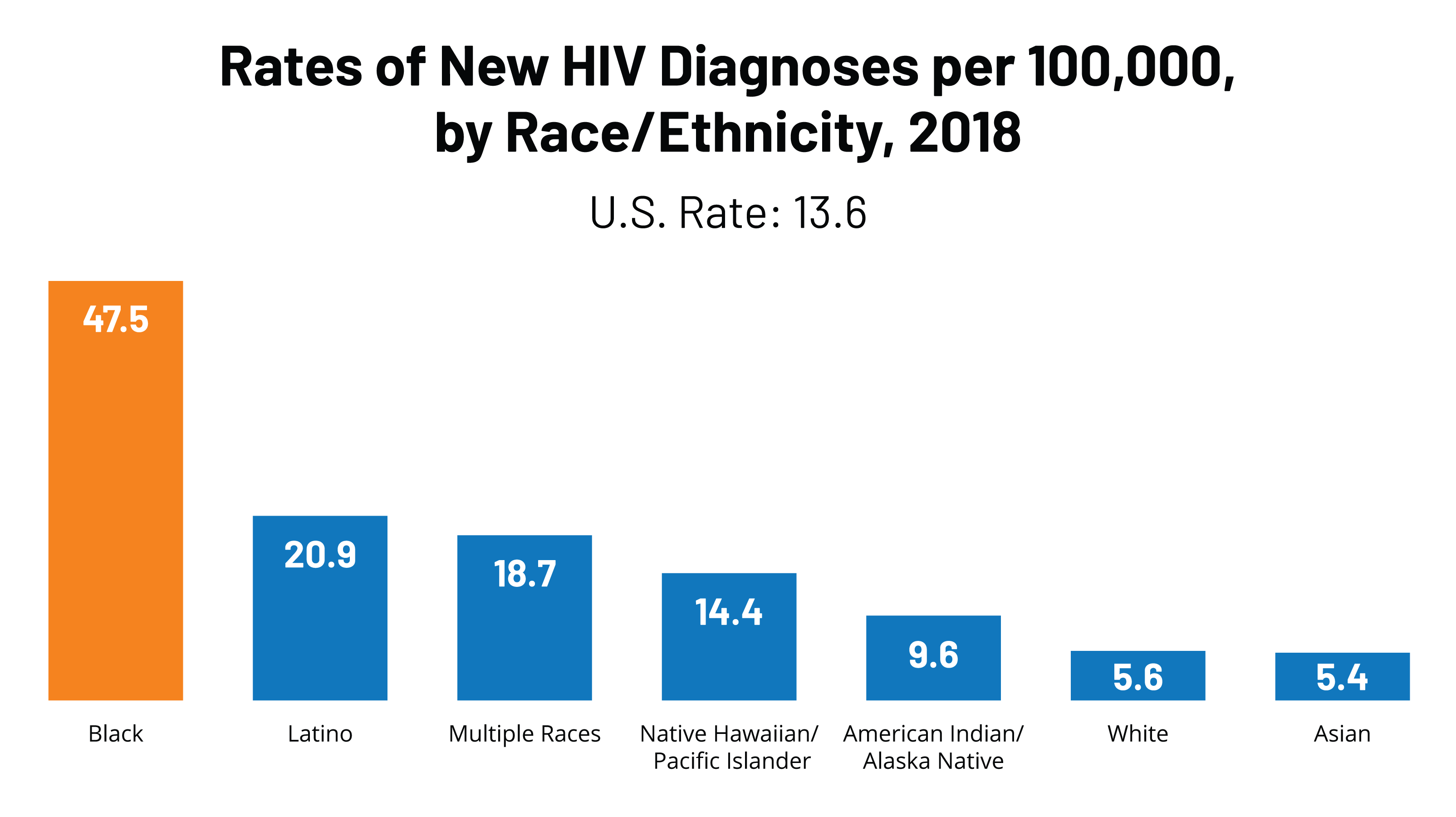 The lack of access to care and rates of poverty highlight and fuel the city’s HIV issue. As it is in the entire country, race is completely connected to poverty in New Orleans. Similarly, “poverty is ideal for the spread of HIV because of the many ways in which it disrupts care” (Wapner). Statistics even show that men of color progress to AIDS five times more often than white people. New Orleans fuels the lack of progress and care for colored men of HIV with the issue of incarceration. Louisiana has the highest incarceration rate in the nation, and New Orleans leads those numbers. “Jail sentences destabilizes home life, which leads to multiple sexual partners, increasing the risk of HIV because so many people living with the disease are either undiagnosed or not in care, enabling viral loads to increase to dangerous levels” (Wapner).
The lack of access to care and rates of poverty highlight and fuel the city’s HIV issue. As it is in the entire country, race is completely connected to poverty in New Orleans. Similarly, “poverty is ideal for the spread of HIV because of the many ways in which it disrupts care” (Wapner). Statistics even show that men of color progress to AIDS five times more often than white people. New Orleans fuels the lack of progress and care for colored men of HIV with the issue of incarceration. Louisiana has the highest incarceration rate in the nation, and New Orleans leads those numbers. “Jail sentences destabilizes home life, which leads to multiple sexual partners, increasing the risk of HIV because so many people living with the disease are either undiagnosed or not in care, enabling viral loads to increase to dangerous levels” (Wapner).
New Orleans has also faced a long history of disasters, causing it to be a face of pity for the nation. There was the aftermath of slavery, Hurricane Katrina, and now the COVID-19 pandemic. Racialized pity detaches the reality of the situation to blame a community on a factor of otherness and the inability to be able to empathize and identify. This issue is another large factor that has created a barrier to effectively decreasing the infection rates of people of color in New Orleans compared to the rest of the country (Balaji).
New Orleans is ground zero for the chance to improvise new queer politics and to employ empathetic strategies to make a difference. There is no reason the rate of HIV infection in men of color should be on the rise in any city. New Orleans has faced many challenges regarding equality and race, and this is one area that needs transformation.
SOURCES
Balaji, Murali. “Racializing Pity: The Haiti Earthquakeand the Plight of ‘‘Others,’’ Critical
Studies in Media Communication Vol 28. No. 1, Taylor & Francis Group. March 2011,
pp. 50-67, https://tulane.instructure.com/courses/2214676/files/folder/12.%20Feb%2015?previe
w=110417883
Poche, Kaylee. “Total HIV Cases Keep Increasing in New Orleans — and Doctors Say That’s
Not a Bad Thing; Here’s Why,” Crescent Care, May 6, 2019,
https://crescentcarehealth.org/total-hiv-cases-keep-increasing-in-new-orleans-and-
doctors-say-thats-not-a-bad-thing-heres-why-gambit/
Villarosa, Linda “America’s Hidden HIV Epidemic,” New York Times Magazine, June 6, 2017,
Wapner, Jessica. “Southern Brew,” Aeon, Pam Weintraub, August 15, 2014,
https://aeon.co/essays/how-new-orleans-became-america-s-ground-zero-for-hiv
This piece was edited by Ethan Meisler as part of Professor Kelley Crawford’s Digital Civic Engagement course at Tulane University.
 NOLAbeings
Multimedia artist Claire Bangser created NOLAbeings as a portrait-based story project that marries...
NOLAbeings
Multimedia artist Claire Bangser created NOLAbeings as a portrait-based story project that marries...
 Data corner: Adobe Suite (create a PDF, social media graphic, presentation, edit a photo and video
Data corner is where you go to work with analytics and top tech skills. It takes on everything from PERL and SQL to Canva and Sprout Social.
Data corner: Adobe Suite (create a PDF, social media graphic, presentation, edit a photo and video
Data corner is where you go to work with analytics and top tech skills. It takes on everything from PERL and SQL to Canva and Sprout Social.
